Achilles tendinopathy
Achilles Tendinopathy

The Achilles tendon attaches your calf muscles including gastrocnemius and soleus to the back of your heel bone ( calcaneus). As you walk, run, and jump, your Achilles acts like a powerful spring, propelling you forward by storing and releasing energy.
Nearly all the force you generate when pushing yourself forward goes through the Achilles tendon. Depending on what research study you read, this force has been reported to be as much as six to twelve times your bodyweight when you’re running fast.
A healthy body is constantly renewing bone and soft tissue ( muscles and tendons) all the time – breaking down old tissue and laying down new stuff.
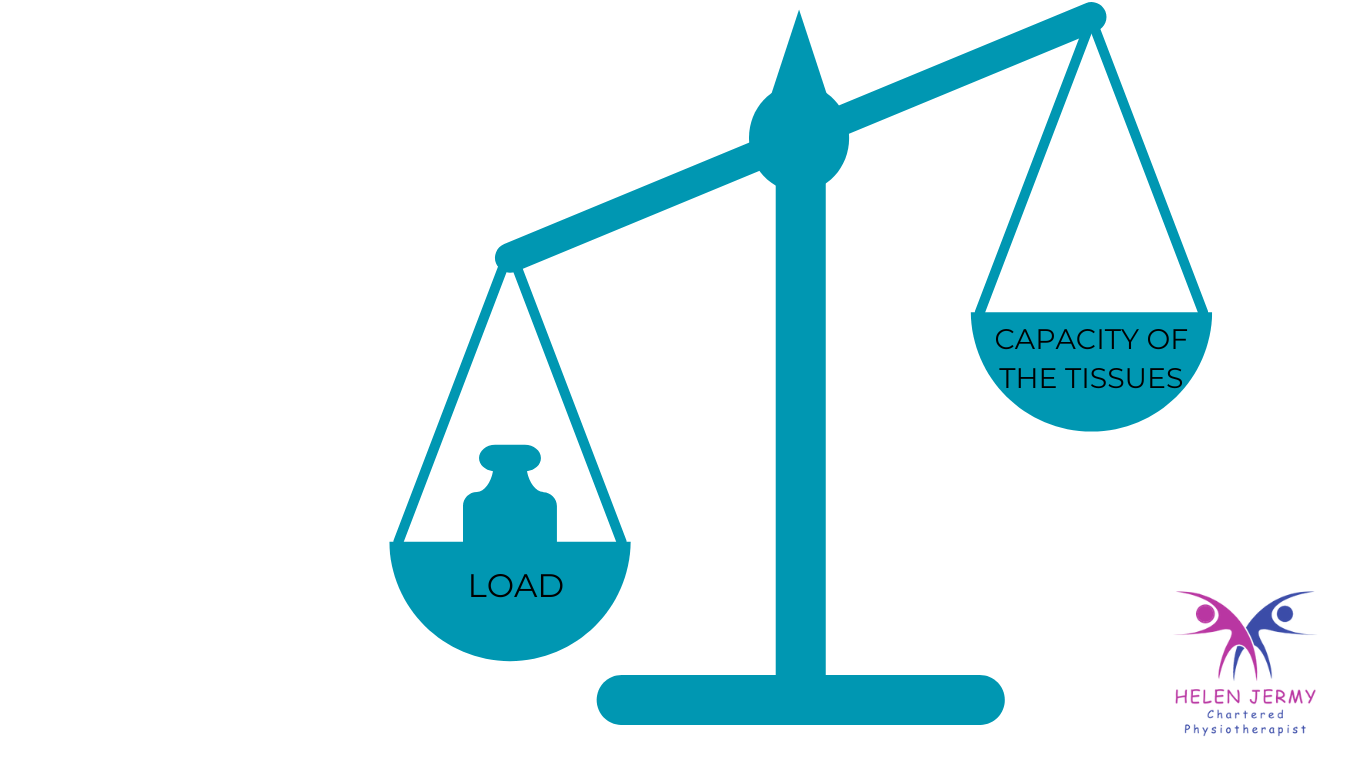
When we exercise and subject our body to greater loads, given time, our body adapts to this increase in load by laying down the new tissue stronger than it was before, and as a result we get stronger and fitter.
However if our body is not given sufficient rest and recovery time to adapt and strengthen the tissue after high intensity and loading activity, the regeneration process can get disrupted and overload / overuse injuries such as Achilles tendinopathy can occur - we have exceeded the capacity of our tissues to withstand load.
Achilles tendinopathy has various causes and is common in active as well as inactive people. For active people the most common cause is overload, while for inactive people it is often linked to certain medication or medical conditions.
Inflammation isn’t always the cause of Achilles tendon pain the term Achilles tendinopathy is now widely used to describe pain in the Achilles tendon.
There are several different stages of Achilles tendinopathy, and consequently the rehabilitation of these are all slightly different, using different exercises and strategies:
- Acute/reactive: New injury, Achilles tendon is thick/swollen, sensitive, sore.
- Disrepair: Pain and symptoms have been grumbling for a few weeks, but often longer, typically painful initially on activity but then improving after a few minutes. The pain is then often worse the following day.
- Degenerative: Chronic Achilles pain, tendon is in a poor condition.
What Causes Overload?
Examples of activities that load the Achilles tendon:
- Walking
- Climbing stairs
- Jogging or running (including running sports like football)
You can overload your tendon in several ways
- Playing sports that require quick changes of direction, lunging, and explosive movements, e.g. hockey, tennis and pickleball.
- Jumping (e.g. basketball, skipping, etc)
- Sudden overload - working the tendon harder than it is used to by rapidly increasing activities such as walking, running and jumping for longer periods of time, or by doing these activities more frequently and or more intensely, or by changing the type of terrain such as adding in hill training rather then flat.
- Gradual overload - not allowing your tendon enough recovery time after training or exercise sessions causing an accumulation of micro-damage
- Suddenly changing your type of foot wear - from heels to flat shoes or using zero drop or minimalist sports shoes increasing the range of movement the tendon has to work through.
- Changing your running style - from heel strike to mid foot or forefoot running increases the load through the achilles tendon, especially if not introduced gradually.
Compression can also overload the Achilles tendon.
The area where the Achilles tendon inserts into the heel bone is naturally compressed against the bone as we move our toes closer to the shin bone (dorsiflexion). Usually this does not cause a problem because, given time, the tendon adapts to withstand the amount of compression caused by our normal activities.
However suddenly increasing the amount of dorsiflexion movements such as sustained ankle and calf stretches, walking uphill, changing to flatter shoes, and holding certain yoga poses can cause a compression overload to the tendon leading to insertional Achilles tendinopathy (less than 2cm from the heel). This is treated slightly differently to mid portion Achilles tendinopathy (2-6cm from the heel) so it is important to identify what area of the tendon is affected during assessment.
There are some other causes of Achilles tendinopathy such as ;
- A direct blow to the tendon
- Perimenopause and Menopause where a drop in oestrogen levels can affect the ability of the Achilles tendon to produce and strengthen collagen fibres which make up the strong rope like tendon.
- Inflammatory conditions such as gout, spondyloarthritis, rheumatoid arthritis, and psoriasis can cause tendon pain that acts in a similar way to tendinopathy
- Diabetes can be a common cause of tendinopathy in inactive people.
- Fluoroquinolone antibiotics can cause severe tendonitis and even tendon ruptures.
- Statins, often prescribed for high cholesterol, may affect a tendon’s ability to produce and strengthen new collagen fibres, leading to tendinopathy.
- A Haglunds deformity ( hard bony lump on the back of the heel bone) may predispose you to getting insertional Achilles tendinopathy, but it is not a direct cause.
Achilles tendinopathy symptoms

The first onset of Achilles pain is often initially felt towards the end of an activity - walk, run, tennis match etc or a perhaps a few hours afterwards. If the tendon has been really overloaded, you may wake up the following morning with a very painful tendon that makes you hobble for most of the day.
If the pain is very sharp and came on suddenly as if you had been kicked in the back of the calf whilst you are exercising you should seek immediate medical attention as you may have torn your Achilles tendon.
It is uncommon to experience visible bruising with Achilles tendinopathy, this may be indicative of a tendon or muscle tear and should also be checked out immediately.
In most cases of Achilles tendinopathy, the Achilles tendon and calf muscles are stiff and/or painful first thing in the morning but then eases once you get up and start to move around. The stiffness may return again if you sit still for too long. The pain can sometimes spread under your heel.
The Achilles tendon is not usually painful in bed or at rest unless there is direct pressure on the injured part of the tendon or you are in a position that stretches the tendon.
Initially, you may find that you feel stiffness and discomfort at the start of a walk or run but that it disappears as the tendon warms up. However, the discomfort and pain may return worse than before a few hours later.
Some people will only feel pain, others only stiffness, and others will have both. It most commonly affects only one leg, but studies have shown that around one in three people develop Achilles pain on both sides at the same time.
The intensity of the symptoms can vary from just a mild discomfort to severe pain and stiffness
There may be a slight lump in the middle of the Achilles tendon or at the heel bone, which is caused by changes in the structure of the tendon rather than true inflammatory swelling. However it is common to also have heel bursitis in combination with Achilles tendinopathy, and you may notice some swelling around the heel bone.
Occasionally especially in older people there may be minimal pain but instead a rather a loss of strength in association with a lump in the
❗️Studies have found that there is no correlation between the intensity of your pain and the amount of damage in your tendon. Pain may tell you that you have an injury, but just because it is very painful does not mean that your tendon is badly injured.❗️
What happens inside an injured Achilles tendon?
A healthy tendon is made up of collagen fibres packed tightly in parallel - this arrangement is what makes a tendon so strong. It also contains some fluid or gel-like substance and some cells between the fibres.
When the injury first occurs to your Achilles tendon, the collagen fibres in the injured part move slightly further away from one another, and you get more fluid and various types of cells between them. At this point, your tendon may feel sore and stiff, but it is usually still pretty strong - the acute or reactive phase.
If you ignore the symptoms and continue to aggravate it allowing the injury to drag on for several weeks or months, the collagen fibres may separate eventually losing their parallel arrangement. This then causes that part of the tendon to lose its strength - the phase of disrepair. The pain may now prevent you from doing your sport and day to day activities and walking may also be painful.
In most cases, it’s only a small part of the tendon that is affected and that the rest of the tendon usually maintains its strength. You can regain your tendon’s full strength by following a treatment plan that usually includes carefully graded rehab exercises.
Common Treatment Options
Load Management:
Load management is the cornerstone of Achilles tendinopathy management.
- Aggravating activities are minimised to allow time for the tendon to heal and for pain to decrease. The activities are then gradually increased until normal function is restored.
Strengthening Exercises Prescribed by Physiotherapist:
Together with load management, strengthening is a core part of Achilles tendinopathy treatment.
- Initially exercises may be isometric, meaning the muscle is contracted, but not lengthened or shortened. Research has shown that not only do isometric exercises increase tendon strength, they also have analgesic effects, and are therefore useful in the early, painful stages of tendinopathy.
- Exercises can then be progressed to a combination of isometric (muscle shortening) , heavy-slow resistance and eccentric (muscle lengthening) exercises. Research has shown that heavy-slow resistance and eccentric exercises increase tendon stiffness and promote realignment of tendon collagen fibres.
- Once these exercises are pain-free, then faster, more activity-related exercises can be slowly introduced, and gradually progressed to plyometrics. This prepares the tendon to deal with a similar amount of energy that it faces when walking, running, or jumping.
- Strengthening may also be necessary in areas further up the kinetic chain - around the hip knee or core, in order to improve the distribution of load, or within the foot to correct postural differences such as over-pronation.
Heat or ice:
- Ice may be used in initial stages and after activity in order to decrease pain.
- Heat may be used before activity and exercise to improve blood-flow and muscle activation.
Massage:
- Massage directly over the tendon may increase pain but may be useful further up the leg in the Gastrocnemius or Soleus, in order to take load off the Achilles.
Dry Needling / Acupuncture:
- Dry needling in the lower leg away from the tendon can be helpful in conjunction with exercise therapy and load management.
Shockwave:
- Shockwave therapy may be used in conjunction with load-management and exercise therapy to improve synthesis of collagen fibres and promote tendon healing.
Heel-Lifts and Orthotics:
- Heel-lifts can be placed in shoes in order to reduce the amount of stretch placed on the achilles tendon during activity.
- Orthotics and heel-lifts may also be used to correct postural imbalances such as decreased range of motion and over-pronation.
The longer you avoid addressing an injury like Achilles tendiopathy, the longer it takes to resolve when you do start with rehab.
If you are suffering with Achilles pain, don’t wait for months hoping it will eventually go away, consult an experienced medical professional and get back on the right track as quickly as possible - rehabilitation may not mean stopping running or your activity but perhaps adjusting it and adding in appropriate loading exercises.
Contact us for more advice or to make an appointment
References:
